You have printed a page containing audio/video content. We can't print that, so we've provided a transcript for you instead.
Conversations with inspectors
Heather - I think the way we view people with dementia is one of the key areas we want to look at and it's about raising expectations. When you go into a service, we want to see absolutely somebody's health and wellbeing needs being met, but we want to see beyond that. We want to see more about quality of life and the kind of meaning we are having for that person. It is looking at their personal outcomes, their goals. That diagnosis of dementia shouldn't be an end to having personal hopes and dreams and wanting to attain things. So it is shifting that and we are saying how that person can actively participate in their own care planning as an equal partner, not as an afterthought. Not when the case review has been done and somebody gets invited in at the end and told 'this is what we have decided for you', but actually right at the beginning. What do you need to make your life have more meaning for you? Have some quality to you? So the outcomes that we are looking for are those that really make a difference to people. Not outcomes for the service, but outcomes for the people who are actually living with that diagnosis of dementia.
Marie - A key area of inspection is looking at participation and how people are involved in their own care. And when people with dementia don't have capacity that can be an issue about how much they can be involved, and how we can promote choice. And sometimes we go to services and people say well I can't have service user meetings because they all have dementia and they wouldn't remember or they make everyone go to a service user meeting. But actually participation is about small, every day choices: would you like to get up now? Would you like a hand with that? It's about getting services to understand that participation isn't just about care plans, or taking part in meetings ... it's about making every day choices and being spoken to in a participative language that allows you to say yes or no that you would like to take part in that.
Marie - An example to me that really brought it home about how important that is, is that one time in a care home I was interviewing a relative. It was a daughter of a service user, and she was an only child. She told me for the first time in her life she hadn't had a birthday card from her mother that year. And that just brought it home to me what it means to be person centred. Her mother had dementia and could not send the card, however if people had thought about her what was important to her and found out what important days for her were, they could have assisted her to have sent a card to her daughter. And its things like that that is really important that we look for in having good outcomes.
Clive - Another scenario that can come along quite often is when someone living with dementia is unable to walk well themselves and they may be forgetting that they cannot walk or that they need their walking aid to walk so that they are not going to fall down if they do get up. Again the care home the service use and relatives need to look at how they can help the person to keep their dependence but at the same time give the care home and the service user the ability to be able to walk or in some cases not. So it all comes back down to good care planning and outcomes planning for the service user with regards to what needs to be in place to protect the service user but at the same time give the staff and give the family the confidence that the person is not going to come to any harm because they do get up, and fall over unfortunately.
Susan - For individual service users, the length of time they are living in care homes and the experience of their life as well is really important. There are lots of ways we can assist and we've had Make every moment count and Make every movement count... we're looking to be living more in care homes and not just existing in care homes. So a lot of the independent living skills promoted by Scottish Government are ones that we would promote as well. And what people can do rather than what they can't do is important for inspectors. When we are present in services we are busy all the time, we are looking and seeing. One of the interesting things for me is that for some staff we're looking at the same things but we are seeing different things within in. And I think the dementia skilled learning resource will highlight what we are looking at and what we actually are seeing. So someone going for a walk- how that can benefit their bone health, their psychological wellbeing, their purposefulness - there are whole elements in there that we can help staff to see so that they can enhance someone's life so that people don't move to a care home to sit in a corner and have a TV in front of them, even if they are not watching it. These subtle bits can make such a difference in someone's live; being able to get out and about, being able to get through doorways, being able to access fresh air in the garden or go out to the shops. Things I take for granted now, and which I'm hoping to take for granted in 10 years' time when I may well be receiving a care home service. And building on all these bits just now will enhance the quality of life for people living in care homes, and who may be living there for quite some time.
Supporting health and wellbeing
Susan - One of the important aspects of supporting people who are living with dementia in care homes is how their medication is used. For some people when they can be distressed then sometimes the medication can feel like first port of call. But that's not our expectation; our expectation is that it would be the last port of call. So one of the aspects that inspectors can pay a lot of attention to is how much medication someone is one, how it's used and how staff use alternative ways of supporting someone. For example, we have in the past looked at life history as a guide to someone's wellbeing. Over the last while there has been more detailed emphasis on if someone is distressed, and what might be causing that- it can be smells, sights, it can be voices, it can be music- playlist for life is there, sometimes local accents can help. There are lots of strategies that we look to see in care plans, because they are just as important ways of supporting someone who is distressed as medication is. The drawbacks of medication of course are all the side effects it can have, how someone can become sleepy, and how that can lead to the physical problems someone can experience. So the pharmacological aspects are important, but just want to reinforce again that they are the last resort and not the first resort and we would look to support staff to follow that through.
Clive - Another area that we come across during inspection with regard to service users' outcomes can be that perhaps a service user that is living with dementia has forgotten that they cannot walk or that their mobility is reduced and they may be prone to having falls. And this causes a challenge obviously for the service user and for the care homes trying to keep the service user safe and also the family obviously not wanting their loved one to get hurt when they try to walk ... So the care home can work clearly with the service user and the family, and try to promote a positive outcome for the resident to ensure that they are able to maintain their life and have positive outcomes, but at the same time are safe. So they can look at information from the Mental Welfare Commission; Rights, Risks and Limits to Freedom, that gives the care home guidance about how to work with people and this can be by risk assessment, or risk benefit analysis, which is looking at the outcomes of the person and how you can try to maintain that person's independence whilst at the same time keep them safe... A way can be, where does the person sit in the daytime? Are they sat so that they can see other people around so that they have reassurance that they are not by themselves, they are not trying to get up if they do then someone can see that they are getting up. Another way is using a pressure area mat so that if this person does get up it sets a call alarm off so staff are aware that the person is moving and again that relates back to having someone there as soon as possible so that the person isn't coming up to any risk of harm but they are still trying to create their own independence.
Susan - For me the benefits of Promoting Excellence is that it highlights for staff that physical care is there in module 3 in the Skilled resource, and it goes on to look at the psychological care and how best to support people. One of the issues for me is that when we are told that people have challenging behaviour, and getting staff to understand that it may be challenging for them but actually it's quite distressing for the service users. It's good that Promoting Excellence is a tool that I can use then to explain that to people, and that brings about better care then I think for the individuals. I think as well for families to understand that if someone's behaviour seems difficult then there is a reason for that, and through complaints but also through inspection we can highlight that for people and use them as tools for explaining. Because a lot of the work we do as regulators is persuading people, it is the interpersonal stuff. All the relationship centred care, that Kitwood talks about and that we've used in systems like SOFI. Brings all that together and helps us with communication, which is one of the main skills a regulator needs. Just to explain to people in different ways how they are working; what the good bits are, but what the bits that aren't so good to us and explaining to them that if they are not good enough for us then why they aren't good enough for the people receiving care, is more important. But we are a conduit that works through all these bits. And again Promoting Excellence has all the guidance that is there, all the signposts and ways to direct people to how they can improve their practice.
Promoting and protecting people's rights
Marie - When we are working or inspecting a service it's really important we keep in mind legislation, not just legislation about care but also overarching legislation like the human rights act and about people's rights under the human rights act - which do not go way if you use a care service, or if you lose capacity. But sometimes those rights can be a tension for people because you can't always meet what everyone wants. Particularly the human rights when people are living in a communal situation. What we need to do it assist services to look at the Scottish Human Rights Association who have done a lot of work with the care sector, and we can use PANEL approach to look at decisions about rights and when or not they are upheld we have to have very clear reasons why they are not upheld. For most people human rights are a fundamental aspect of all our lives and should not be taken away from us because we go into care.
Marie - There is lots of new technology out there which allows people to live in their own home rather than going into a care home. For example, you can turn off someone's cooker so they can't burn themselves and someone coming in to do their meals. You can also have buzzers for medication, so a reminder goes off and says take your medication and gives people that reminder. If the front door is opened and someone goes out at night an alert system can go to the local authority who will know that person and they will have written down routes that that person will normally take and they can send someone to intercept them and bring them home so that person is safe. So there is lots of technology out there that we can use that is becoming increasingly used to keep people at home, and in care homes as well we are starting to see the use of some technology. Some of the concerns that I have with technology are about the ethics of it and the sorts of technology we are using. An example is CCTV throughout care homes where everyone's every minute it monitored, how would we like that? And it's interesting that a large provider in the UK has just done a survey about using CCTV throughout their services. And relatives were really in favour of it but actually residents have said no, they do not want to be on camera all the time. So there are bits when you can keep people on camera for certain amounts of time, but you need to ensure people's right to privacy, to be treated with dignity and to not have everything filmed is there. So there are ethics around it, and it's time we have a discussion around where that comes in, when is the right time to use technology and when it isn't.
Clive - Another aspect the role of the inspector is to inspect and regulate services in the community. This can be inspecting care at home services; people living in their own homes that have someone come in to help and support them, or attending a day centre where they go into a formal establishment and have staff to support them during the day. The important thing here in both situations is that we ensure that the person is able to live independently, have their own rights, be protected, and that the service that is provided is meeting the care needs that they wish to have and ensuring the care planning information that is provided meets in with the dementia standards and obviously the national care standards that we work with as well... It's important that the service user feels that the care that is being provided to them is what they need and they wish. And this is essential when it comes to care planning, especially when they are being supported with personal care etc., that all the staff members who go into attend to that person know how that person wishes their care to be provided. And they are then protected, and ensured that they are receiving the best care possible.
Heather - We know that dementia doesn't just affect the person living with dementia, it affects the whole family, it affects your friends, it affects your neighbours, where you live so that it extends further, so I think we have to be really careful and really think about the needs of the person with dementia first and foremost and that is not to say we put he needs of the family or carers second, but is to think of people with dementia as citizens in their own right. I think there has been a move to think of people with a cognitive impairment or any kind of, memory problem with not having the full rights of citizenship and for them and maybe for them some of the basic human rights are not applicable to them, we know within the Care Inspectorate that this is not the case, we are very strongly upholding peoples Human Rights within all the services that they receive, but also within society as a whole, we are seeing people coming through, living with dementia who are taking the role of activist of leaders within the community. If we think about the Scottish Dementia Working Group, they were involved at the very first stages of drafting the dementia strategy, the standards, their voice ringing loud and clear throughout all these principles, so it's really important that's the voice we hear first. Now there's sometimes becomes issues where maybe their views of the person with dementia could be at odds with the families and carers and they are living with and a lot of that is around risk. It's understandable, there's lots of risk involved when somebody starts to develop dementia, there's worries that the family can have, but sometimes those risks, the risk of physical harm get the greatest level of priority, so we are very worried about people getting lost, we are worried about people falling over, but we are less worried about what we could call the silent harms, we are less worried about the frustration that comes about because their independence has been taken away, about agitation that comes as a result of having a locked door constantly when you are trying to go somewhere where you want to go, so I think it is really important is that when we look at risk and are working with families and carers and the person with dementia that everybody gets an opportunity to have their say and I suppose one voice is not louder than any other, but we always have to come back to that person who is living with dementia. Looking at their needs, what matters most to them is the crucial part here.
Joe - The Standards of Care for Dementia in Scotland are very useful because they help the public to understand the expectations placed on care services looking after people with dementia, but also it highlights that we expect a lot more than we did in the past. So for example, care services often have locks on the doors. And yes we have locks on our own house doors. But it's about allowing people to have freedom of movement, to come and go as they please and this also related to national care standards that highlight this. So standards are really important because it helps people to be absolutely crystal clear about what expectations people can have. All too often expectations are lower than they should be ... Which brings me to co-regulation. Because if we are relying on the public to be our eyes and our ears it's really important to understand what standards we can expect. If they are expecting less then they are not going to raise issues or come to us with concerns, because they are going to be thinking this is ok, when very often it isn't ok and we need to push services to be the best that they can be. So that people's rights can be respected and people can do what they really want to do when they are using a service... within reason.
"People with dementia and their carers have the right to full participation in care needs assessment, planning, deciding and arranging care, support and treatment, including advanced decision making."
Charter of Rights for People with Dementia and their Carers in Scotland (2009)
The national focus on personal outcomes approaches in health and social services aligns well with the above statement from the Charter of Rights for People with Dementia and their Carers in Scotland (2009). It aligns well because its aim is to shift engagement with people who use services away from service-led approaches and towards personalised, person centred solutions.
In light of this, personal outcomes, family oriented care and community connections are central to the ethos and philosophy of practice as we go forward. This involves people with dementia and those closest to them working in partnership with professionals, services and communities to identify what matters to them, and to choose how services and supports can be best employed in maintaining or strengthening their wellbeing. In best practice, the strengths, capacity and resilience of people using a service are recognised and promoted, building upon natural support systems and much wider community based resources, so that the best possible impact is made on every person's life.
"What I would say to the professionals is that - you can pull me back, give me my life back and pull me into the light. And by the same token, ignorance, arrogance and couldn't care less, you can shove me down into the darkness and just cast me away. I can't do it, I need your help to do it."
Through our eyes , a life with dementia Scottish Dementia Working Group
Past, present and future initiatives promoted by the national dementia strategies serve as illustrations for how personal outcomes, family oriented care and community connections are becoming embedded in practice. For example, in 2014 the Alzheimer Scotland eight pillar model of community support inspired a pilot project across five community health partnerships in Scotland. You can read more about this and how Scotland is developing its capacities more widely in delivering post diagnostic support by visiting the Focus on Dementia website (and others highlighted in Key resources). The following eight pillars quote from Kinnaird (2012) captures how one such national initiative is championing community connections and family oriented care:
Assisting people with dementia and their carers to maintain and build on their existing social networks and identify opportunities for peer support can enhance their quality of life. It can also maximise the natural support received from those around them. It can help people to attain and maintain maximum independence and have full inclusion and participation in all aspects of their life.
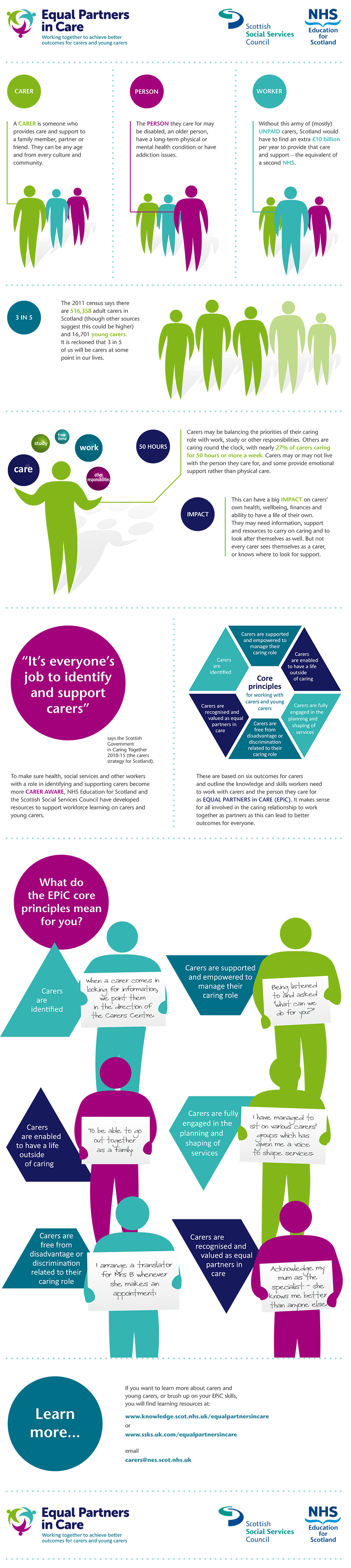
An awareness of the carer's strategy Caring Together (2010-2015) will support you to further understand the importance of working with families and carers as equal partners as we go forward. Unpaid carers, the focus of this strategy, are much more than part of a support system; they are sources of shared experience and identity. Their on-going involvement helps the person with dementia to retain their sense of identity and belonging, however the caring role can have a profound effect. Carers often describe a sense of loss and feelings of distress. Those in regulatory roles can significantly increase awareness of the impact of the caring role, and how this awareness can be coupled with better carer involvement and wider family support to make meaningful changes in service provision and quality of life for each member of the caring relationship. The Equal Partners in Care (EPiC) Core Principles for Working with Carers and Young Carers illustrate best practice. The EPiC framework and accompanying learning resources can be highlighted to services, and you are also encouraged to access the EPiC website to complement your carer-focused learning from this resource.
Within your inspection role, the Dementia Standards and the Promoting Excellence Quality of Life outcome indicators will be vital tools. They can support you to detect and evaluate elements of practice from a variety of perspectives, including community connectedness and the degree to which families and carers of people with dementia are enabled to take roles as partners in care. One outcome indicator for example states:
People with dementia, their families, friends and carers, have access to the information, education and support that enhances the wellbeing of the person with dementia and those that support them.
You can find the outcome indicators, and their relation to the Dementia Standards, within the Promoting Excellence learning framework and they will be referred to throughout this resource.
You should now access a range of existing learning resources and further reading. We have highlighted some key resources for you already. Alongside key reading, you can use the Developing your practice and Voices of experience films and activities within this section to support you to achieve the learning outcomes.
Click to download this image as a PDF