Click to download this image as a PDF


You have printed a page containing audio/video content. We can't print that, so we've provided a transcript for you instead.
Susan - One of the important aspects of supporting people who are living with dementia in care homes is how their medication is used. For some people when they can be distressed then sometimes the medication can feel like first port of call. But that's not our expectation; our expectation is that it would be the last port of call. So one of the aspects that inspectors can pay a lot of attention to is how much medication someone is one, how it's used and how staff use alternative ways of supporting someone. For example, we have in the past looked at life history as a guide to someone's wellbeing. Over the last while there has been more detailed emphasis on if someone is distressed, and what might be causing that- it can be smells, sights, it can be voices, it can be music- playlist for life is there, sometimes local accents can help. There are lots of strategies that we look to see in care plans, because they are just as important ways of supporting someone who is distressed as medication is. The drawbacks of medication of course are all the side effects it can have, how someone can become sleepy, and how that can lead to the physical problems someone can experience. So the pharmacological aspects are important, but just want to reinforce again that they are the last resort and not the first resort and we would look to support staff to follow that through.
Clive - Another area that we come across during inspection with regard to service users' outcomes can be that perhaps a service user that is living with dementia has forgotten that they cannot walk or that their mobility is reduced and they may be prone to having falls. And this causes a challenge obviously for the service user and for the care homes trying to keep the service user safe and also the family obviously not wanting their loved one to get hurt when they try to walk ... So the care home can work clearly with the service user and the family, and try to promote a positive outcome for the resident to ensure that they are able to maintain their life and have positive outcomes, but at the same time are safe. So they can look at information from the Mental Welfare Commission; Rights, Risks and Limits to Freedom, that gives the care home guidance about how to work with people and this can be by risk assessment, or risk benefit analysis, which is looking at the outcomes of the person and how you can try to maintain that person's independence whilst at the same time keep them safe... A way can be, where does the person sit in the daytime? Are they sat so that they can see other people around so that they have reassurance that they are not by themselves, they are not trying to get up if they do then someone can see that they are getting up. Another way is using a pressure area mat so that if this person does get up it sets a call alarm off so staff are aware that the person is moving and again that relates back to having someone there as soon as possible so that the person isn't coming up to any risk of harm but they are still trying to create their own independence.
Susan - For me the benefits of Promoting Excellence is that it highlights for staff that physical care is there in module 3 in the Skilled resource, and it goes on to look at the psychological care and how best to support people. One of the issues for me is that when we are told that people have challenging behaviour, and getting staff to understand that it may be challenging for them but actually it's quite distressing for the service users. It's good that Promoting Excellence is a tool that I can use then to explain that to people, and that brings about better care then I think for the individuals. I think as well for families to understand that if someone's behaviour seems difficult then there is a reason for that, and through complaints but also through inspection we can highlight that for people and use them as tools for explaining. Because a lot of the work we do as regulators is persuading people, it is the interpersonal stuff. All the relationship centred care, that Kitwood talks about and that we've used in systems like SOFI. Brings all that together and helps us with communication, which is one of the main skills a regulator needs. Just to explain to people in different ways how they are working; what the good bits are, but what the bits that aren't so good to us and explaining to them that if they are not good enough for us then why they aren't good enough for the people receiving care, is more important. But we are a conduit that works through all these bits. And again Promoting Excellence has all the guidance that is there, all the signposts and ways to direct people to how they can improve their practice.
Health promotion is the process of enabling people to increase control over, and to improve, their health. To reach a state of complete physical, mental and social well-being, an individual or group must be able to identify and to realize aspirations, to satisfy needs, and to change or cope with the environment. Health is, therefore, seen as a resource for everyday life, not the objective of living. Health is a positive concept emphasizing social and personal resources, as well as physical capacities. Therefore, health promotion is not just the responsibility of the health sector, but goes beyond healthy life-styles to well-being.
Ottowa Charter for Health Promotion
The excerpt above, from the Ottowa Charter, describes health as a resource for everyday life. It recognises the responsibilities we all hold in promoting and supporting health and wellbeing, while also echoing the ethos of approaches which reinforce strengths, resilience and existing personal resources. Promoting Excellence (2011), the Charter of Rights for People with Dementia and their Carers in Scotland (2009), and the Dementia Standards (2011) mirror this ethos of seeing whole throughout and ensure people with dementia are aware of the expectations they should have of services. For example one standard states:
"I have the right to access a range of treatment, care and supports"
These publications, and many others that have emanated from the dementia strategies, are based on human rights and have broad support across Scotland, reminding professionals and communities alike that people with dementia have the right to health care and broader social and emotional support which takes into account the context of their entire lives, and never primarily or solely their dementia. As you work through this section and explore the testimonies and range of existing resources, you will have the opportunity to enrich your existing knowledge; strengthening your confidence in recognising good and poor practice in promoting health and wellbeing for people with dementia in care and support settings, and in sharing tools and strategies with the services that need to work towards improvement.
Services have long been able to access information to support them to develop knowledge and skills in working with people with dementia. Quality learning resources have been available, often free of charge, from a variety of institutions and it is clear that there are growing areas of better practice across Scotland, however good practice is not yet universal practice. People living with dementia need workers across health and social services who have a detailed understanding of how dementia affects them, and who not only recognise the importance of a range of health care treatments alongside social supports but furthermore know how to access or instigate them. Some recent reports and publications remind us where we have come from, and how far we need to go. Prior to the publication of Scotland's first National Dementia Strategy, the Care Inspectorate (then Care Commission) and the Mental Welfare Commission for Scotland published Remember I'm Still Me, a joint report on the quality of care for people living with dementia in Scottish care homes. Included below are some key findings.

Living well and experiencing a good quality of life is an important and permanent priority for all of us. However, for a number of reaons people living with dementia can find it increasingly difficult to maintain this quality of life. This situation can be worsened if services and supports are not designed and planned around specific needs and choices, including what matters to the person as their dementia progresses. It is also common for family members and carers to experience severe distress in such circumstances.
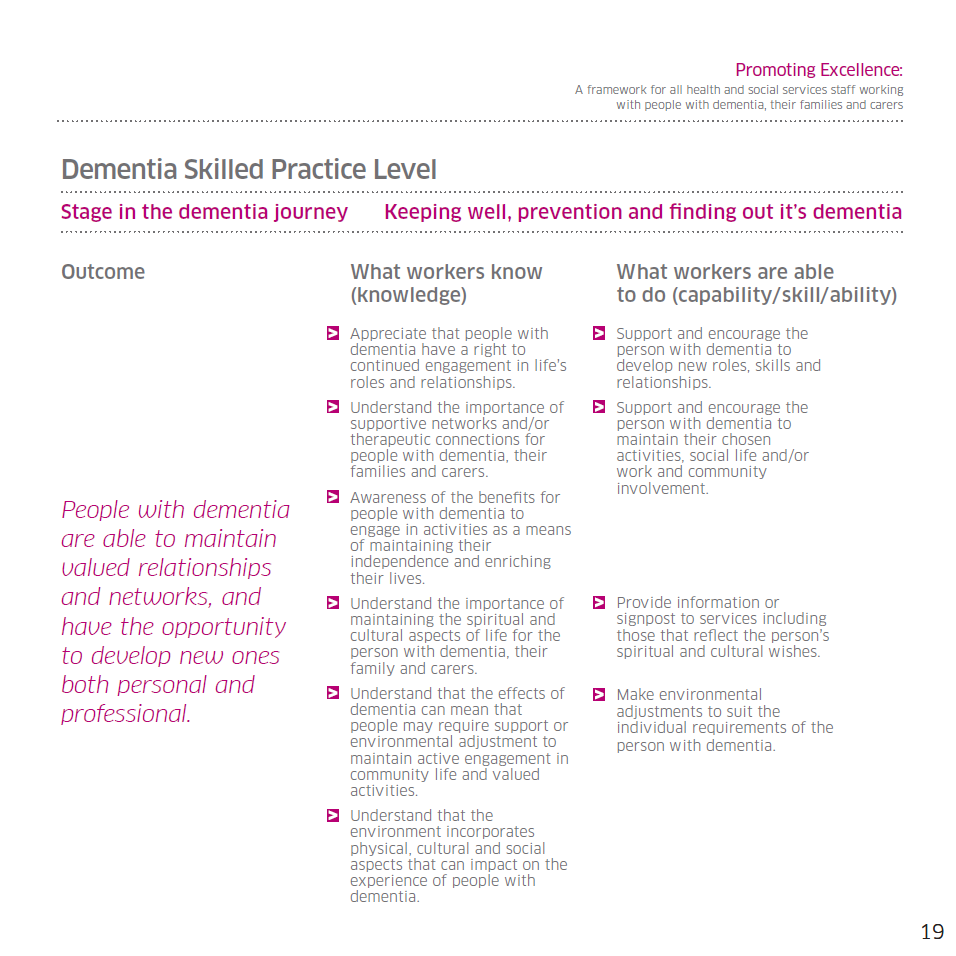
Promoting Excellence brings attention to the journey, defined below, and is structured to take this and the subsequent expectations placed on a worker's knowledge and skills into account. Knowledge of the framework can therefore support you to prepare services, and direct them towards improvement.
Click on the stage titles below to see examples of the knowledge and skills defined for workers at the skilled to enhanced levels of practice.
As discussed elsewhere in this resource, a recommended way of using Promoting Excellence in practice to effect positive change is to work with services and increase their familiarity with the framework's Quality of Life outcome indicators.There are tools and approaches available to support this, and you should liaise with your colleagues to access these and share experiences. Outcome indicators are integral to how the Promoting Excellence knowledge and skills framework is structured, and encourage services to consider the impact of the support and care they provide against specific themes which were developed from a literature review and which are relatable to the Dementia Standards. One specific outcome indicator in Promoting Excellence states:
"People with dementia maintain their best level of physical, mental, social and emotional wellbeing."
As an inspector, you have a significant part to play in making this a reality.