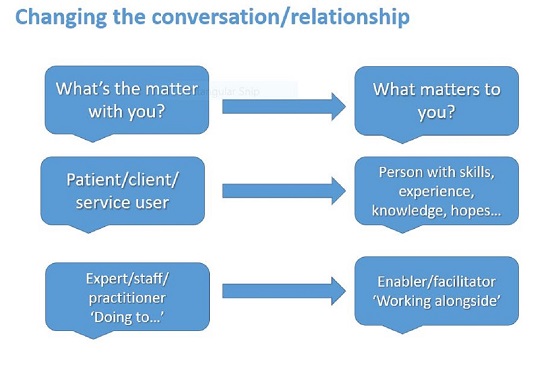
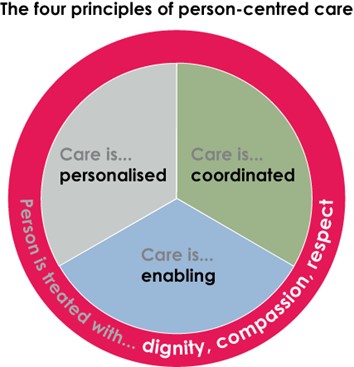
There is no single definition for the term ‘person-centred’. There are many ways in which it can be practiced. It is generally agreed however that there are common principles underpinning this approach.
The Health Foundation's person-centred care made simple provides an overview of how person-centred care supports people to develop their knowledge, skills and confidence.
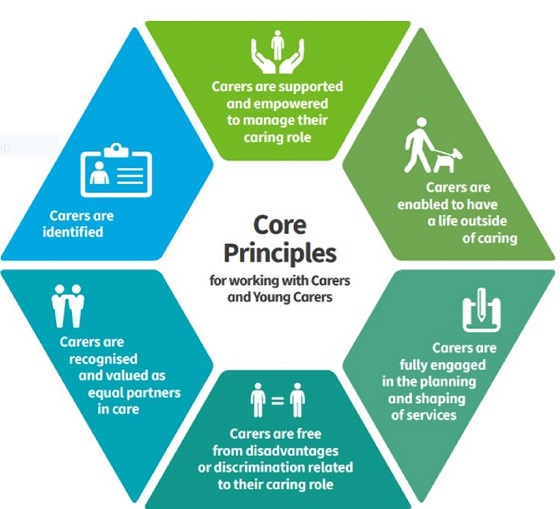
Principles which underpin person-care are:
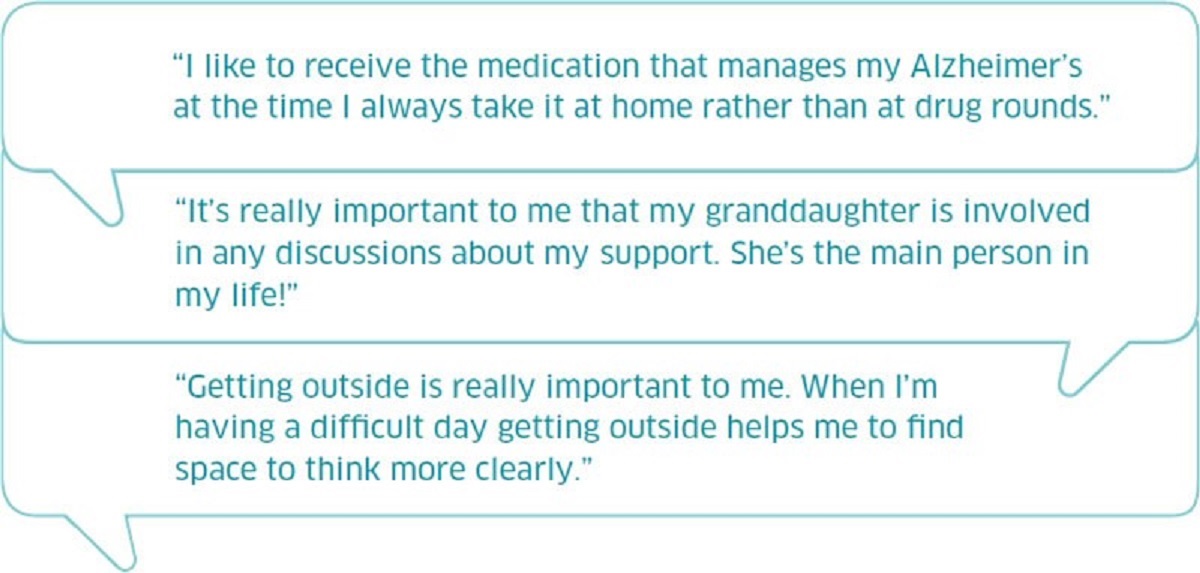
- affording people dignity, compassion and respect
- offering coordinated care, support or treatment
- offering personalised care, support or treatment
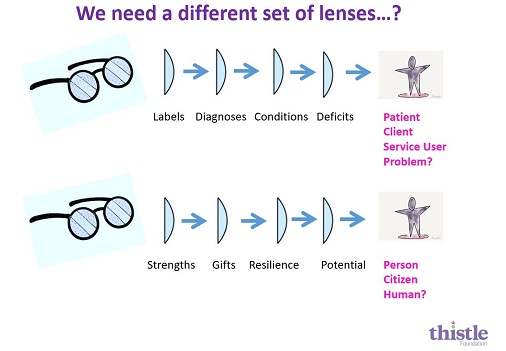
- supporting people to recognise and develop their own strengths and abilities to enable them to live an independent and fulfilling life.